Reviewed by Abbie Jacobs, RN, BSN
Odds are, when you decided to become a nurse, you picked a nearby nursing school and got your degree. Then you got your license in the same state you were already living in and got a job in the same area.
Now you’re ready to make your next move: getting a master’s degree and becoming an advanced practice registered nurse (APRN).
You have to start thinking strategically when you are ready to move up the chain to become an APRN, though. Unlike registered nursing, there are few things that are standardized between states for NPs and other APRNs. This means you need to become familiar with the state of the profession and the specific regs in your state for a real understanding of what your work is going to look like.
These differences will have a big impact on what the job is like day to day, affecting everything from your professional autonomy to your ability to write prescriptions, to the availability of jobs and how much you can expect to earn.
So before you chart out your future career, here’s the top five things you need to know about for the right expectations of what your career as an NP or other APRN is going to be like.
We give you the quick answers you’re looking for to those big questions, along with the resources you need to dig deeper.
Supervision Requirements
One of the widest ways that states vary in their handling of nurse practitioner licensing is in supervisory requirements and physician collaboration. Independence is one thing you’re probably looking for as a nurse practitioner, but if you’re licensed in a state with strict supervisory requirements, you’re not going to get it.
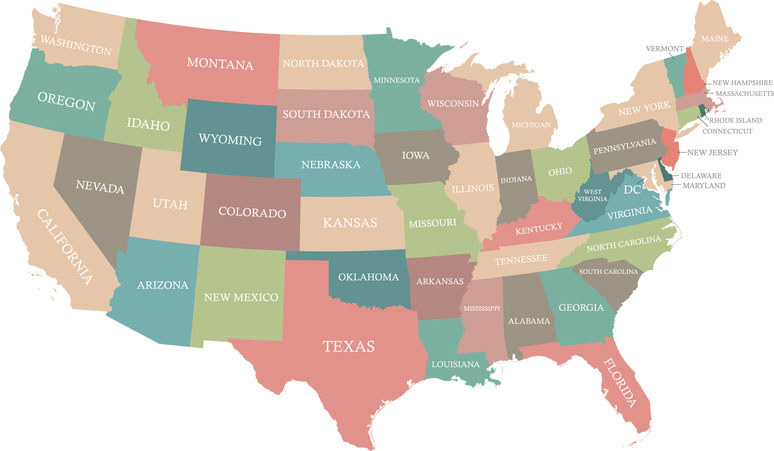
All states fall into one of three categories: 1) Full Practice States – those that allow APRNs full independent authority with no requirements for physician oversight, 2) Restricted Practice States– those that require an official collaborative agreement and direct on-premises physician oversight of all activities, 3) Reduced Practice States– those that allow NPs and other APRNs a certain level of autonomy, but that still require a collaborative agreement with a physician, which may only be limited to diagnosing and prescribing activities, and which may only require a phone consultation rather than on-premises oversight.
The American Association of Nurse Practitioners has a convenient state-by-state breakdown that will help you better understand the requirements in your state when it comes to physician oversight.
Salary and Benefits
Nurse practitioners make more than nurses everywhere, but not always as much more as you would think. In some regions, the average salary is well below the average national pay for NPs of $91,450. And even that number looks low if you compare it to places like Alaska, where they earn a whopping $112,090 on average.
It’s easy to check salary from the Bureau of Labor Statistics for nurse practitioners, but why go that far? We’ve already done the digging for you and compiled average salary information by state right on this website.
Prescriptive Authority
Not all nurse practitioners are in roles where they want or need to prescribe medications. But if you are, then you need to take a close look at the regulations surrounding prescriptive authority. In some cases, this can be even more limiting than physician supervisory requirements. You may need a physician’s authority to prescribe certain drugs, and can be prohibited from offering others entirely.
State regulations on prescriptive authority typically align with rules on physician oversight and collaborative agreement, but some important differences exist state to state. Some states allow full, unrestricted prescriptive authority… others only allow NPs and other APRNs to prescribe under direct physician oversight, in which case the prescription is filled through the MDs FDA number with the doctor ultimately bearing the responsibility for the prescription… while others may restrict the types of medication and pharmacologic therapies an NP or other APRN is allowed to prescribe independently.
The scoring grid the National Council of State Boards of Nursing (NCBSBN) uses to track the degree to which each state is aligned with the APRN Consensus Model provides a state-by-state breakdown of the specifics surrounding state regs related to writing prescriptions.
Demand for Practitioners
In some sense, APRNs working today or graduating soon don’t have much concern about demand for their services. With a looming shortage of doctors (the American Association of Medical Colleges predicts there will be 100,000 empty physician positions by 2030) on the horizon, almost every state is going to find itself strapped for primary care providers for the foreseeable future.
But these trends and the extent of the demand can differ around the country. Alaska, for example, has long been a mecca for APRNs, with high pay rates and liberal rules regarding licensing and autonomy. But, according to the Alaska Department of Labor and Workforce Development, in recent years the state’s population growth has flattened. As a result, job growth projections remain low, and the baby boomer retirement bump expected to boost the need for medical care throughout the United States, may also be flatter there.
To get a feel for the job growth rate for NPs and other APRNs in your state, you’ll need to look at a resource from outside the nursing community. This US Department of Labor sponsored resource for Long Term Occupational Projections gives you details on the current number of NPs, nurse-midwives and other APRNs licensed in your state, and how many new jobs are expected to become available in the years ahead.
Future of the Profession
One thing about all of these licensing issues is that they are subject to change. It’s only been since the 1990s that nurse practitioners have widely enjoyed these benefits and authorities in any states at all. The pursuit of professional autonomy and independent authority to practice and prescribe to the full extent of their training and education has been slowly gaining ground state by state. Today’s limitations may not exist in another five or ten years, depending on where you are considering getting licensed.
It’s worth looking into the progress of legislative efforts toward full practice autonomy and prescriptive authority in those states. The APRN Consensus Model Implementation Status interactive map give you a way of tracking those developments in near real time, showing you which states are fully aligned with the Consensus Model that allows full independent practice authority, those that haven’t begun moving in that direction at all, and all the states in between that have taken at least a step or two toward making independent practice law within their borders.